Blue light cosmetic tests
Exposition to digital pollution is a growing concern among cosmetic products consumers. Such pollution comes from screens (smartphones, tablets, computers…) which are now omnipresent in our daily lives. Digital pollution results from the blue light emitted by screens and is now known to be harmful for eyes and quality of sleep. Human skin is exposed to blue light as well, and it is a trending topic in the cosmetic industry. Indeed, innovative cosmetic products are developed to prevent the damages caused on skin by blue light exposure. As a consequence, the industry need to rely on innovative blue light cosmetic tests to support this claim.
Syntivia uses a skin cell model to carry out solid cosmetic tests. We developed a blue light irradiation dose corresponding to 1h to 2h40 of screen exposure. It allows us to test and validate cosmetic product’s efficacy against blue light-induced skin damages.
Cellular model: primary cells in culture
Proper conditions allow cells in culture to live, grow and maintain their functions as if they were within the skin. Syntivia uses primary cells, Normal Human Epidermal Keratinocytes (NHEK) in 2D culture. Cells are isolated from skin epidermis ans kept growing under adequate conditions to reproduce the human skin configuration.
Our equipment allows us to obtain reliable results on this model by analyzing:
- Cell viability
- Biomarkers involved in skin water balance
- DNA damages signaling
- Senescence
Effects of blue light on skin cells
We developed two conditions of blue light exposure with increasing doses: single or chronic irradiations. Based on this model and these conditions, we carried out various tests. Both models are of interest:
- Single irradiation rapidly generates lesions. This condition is interesting to test products that immediatly protect the skin.
- Chronic irradiation mimics closely the reality of skin exposed to blue light on a daily basis. The effects induced by this condition are more important than those of a single irradiation. This condition allows to test products that will have a long-term effect.
The various parameters analyzed allow to measure the increasing protection power of cosmetic active ingredients.
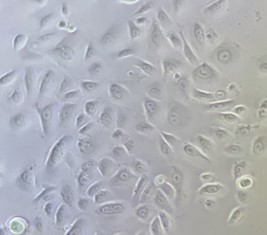
Effect of blue light on cell viability
A viability test was carried out on NHEK exposed in a single or chronic way to blue light. This allows to identify the cytotoxic dose in both conditions.
Viability test after a single exposure (left) and after chonic exposure (right) to blue light irradiation. Increasing irradiation doses were tested.
The cell viability is inversely proportional to the dose of blue light applied.
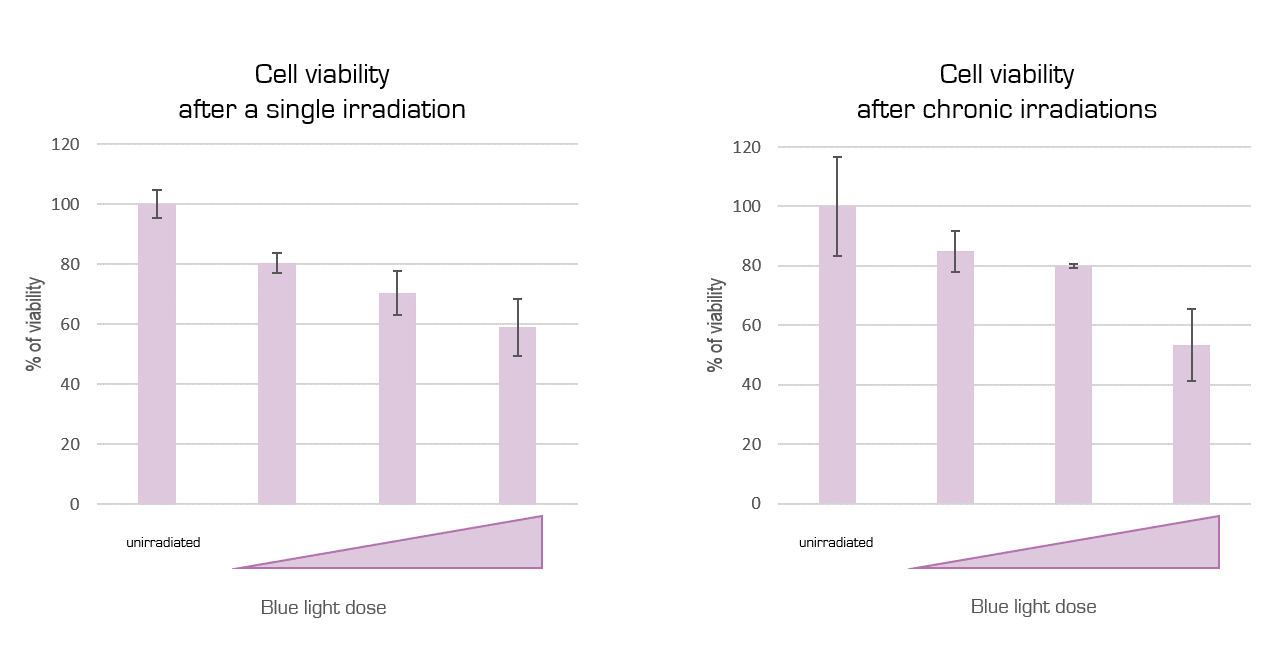
Effect of blue light on DNA in skin cells
Epidermal cells were exposed to various doses of blue light and γ-H2AX expression, a marker of DNA damage [1], was detected by immunofluorescence and quantified.
γ-H2AX immunofluorescence detection by fluorescence microscopy on unirradiated NHEK (left) and irradiated NHEK (right). Cell nucleus are labelled in blue and γ-H2AX in red.
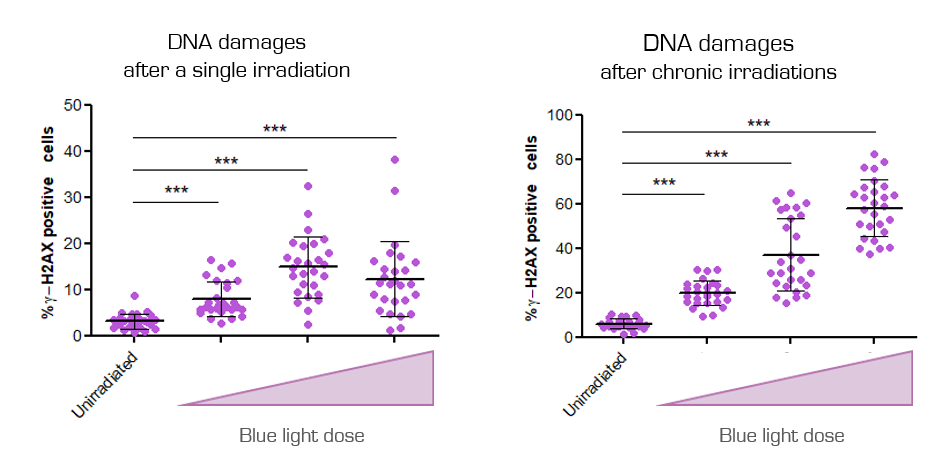
γ-H2AX labelling quantification after a single irradiation (left) and after chronic irradiations (right). Increading irradiation doses were tested.
Cells irradiated with increasing doses of blue light (once or three times) clearly show an increase of γ-H2AX expression, proof of DNA damages.
Effect of blue light on skin water balance
Epidermal cells were irradiated with blue light at various doses and Aquaporin 3 expression, hydration marker [2], was detected by immunofluorescence and quantified.
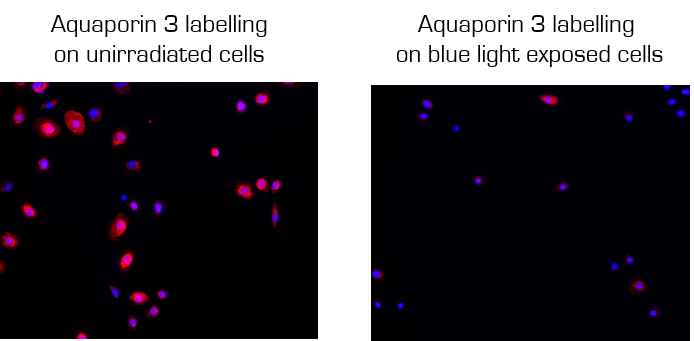
Aquaporin 3 immunofluorescence detection by fluorescence microscopy on unirradiated NHEK (left) and irradiated NHEK (right). Cell nucleus are labelled in blue and Aquaporin 3 in red.
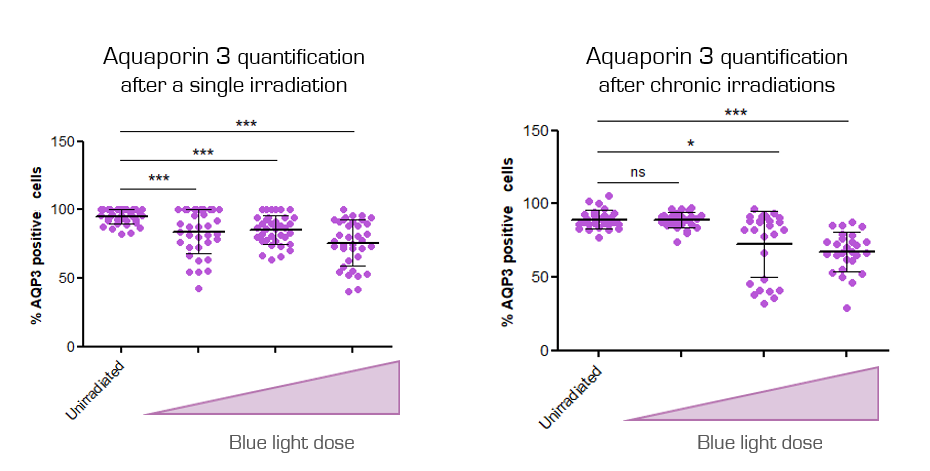
Aquaporine 3 quantification after a single irradiation (left) and after chronic irradiations (right). Increasing irradiation doses were tested.
Exposure to blue light reduces the expression of Aquaporin 3, demonstrating the impact of this stress on the skin’s water balance.
Effect of blue light on cell senescence
After exposure to blue light, Lipofuscin, a marker of cellular senescence [3], was labelled with Sudan Black B coloration and observed with an optical microscope with transmitted light coupled to a colour camera.
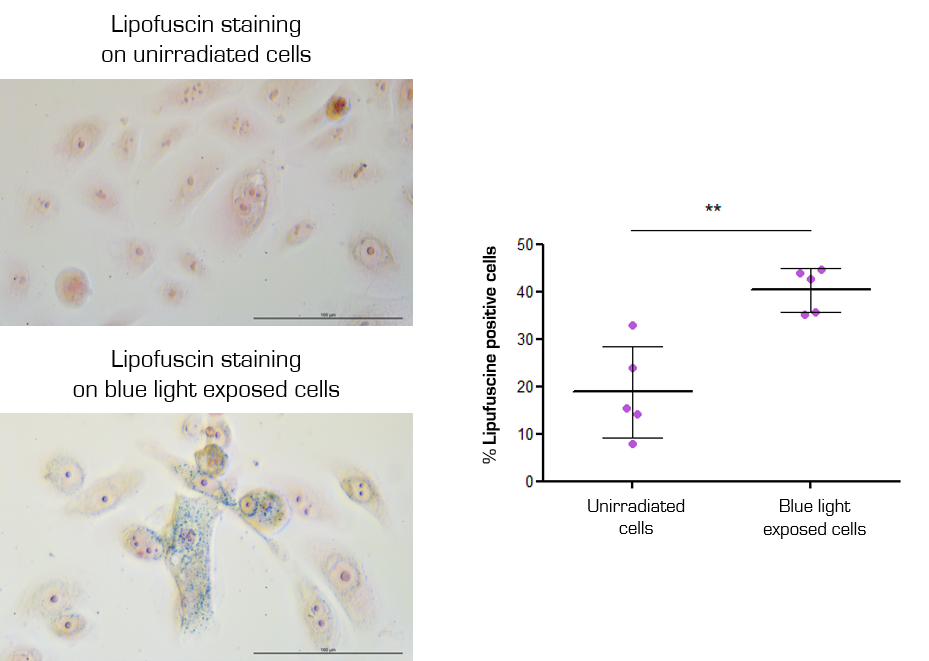
Lipofuscin staining and quantification on unirradiated NHEK and after chronic irradiations with the highest blue light dose (right). Cell nucleus are in pink and lipofuscin in blue.
Keratinocytes chronically exposed to blue light become senescent, as shown by the lipofuscin staining. Cell senescence induces skin’s premature aging.
NB: A same activation of senescence was measured on Normal Human Dermal Fibroblasts (NHDF) exposed to blue light.
Our cell model is hightly sensitive to blue light and perfectly adapted to evaluate cosmetic active ingredients
Blue light irradiation results in loss of viability, emergence of DNA damages, unbalanced skin moisture, and senescent cells. These effects can be countered to precisely define your product’s cosmetic claims regarding protection against blue light damages.
What’s next?
Studies are currently running to validate ex vivo models to carry out blue light cosmetic tests on skin explants. Do not hesitate to share your projects with us so that we can set up a study adapted to your needs.
Sources :